Menopause Supplements
Katrina Borthwick - 20th January 2026
Introduction
As a woman of a ‘certain age’, I am finding that as I scroll through social media I am being ambushed by sponsored posts promising to “banish hot flashes for good” and “restore youthful balance with one natural pill a day” or, more recently, “balance my cortisol”. It seems I’m not alone.
The internet is overflowing with miracle menopause supplements making promises to cure all my ills. Between pastel-toned Facebook ads and in-game adverts offering the secret to “natural hormone harmony,” it’s easy to wonder - are these little bottles full of botanical wizardry, or just expensive hype with a fancy hashtag? In this article, I’ll sift through the marketing sparkle and find out if any of these social-media-famous potions actually deliver, or if they’re just trending for all the wrong reasons.
‘Natural’ hormones
First things first: a little lesson on hormones.
Progesterone is important for protecting the uterus lining if you take oestrogen. That’s why people taking oestrogen as hormone replacement therapy will be prescribed progesterone as well. Inadequate or fake ‘progesterone’ can increase the risk of this lining thickening, causing bleeding or even cancer. This is one reason why medical guidelines do not recommend ‘natural’ supplements for menopause treatment. If you get it wrong, for example taking ‘natural’ progesterone alongside prescription oestrogen, it can harm you.
There are also other safety risks. The content of these supplements is unregulated, so you don’t know what you are getting. Along with that, there is a possibility the contents are contaminated with other ingredients, a risk of drug interactions and, worryingly, such supplements may also mask the symptoms of real hormonal disorders that need to be checked out properly.
Soy
Although it is claimed that the phytoestrogens in soy isoflavones can weakly mimic oestrogen, the only evidence is that it possibly has some cholesterol-lowering effects. Most studies have not shown consistent or significant benefits for symptoms such as hot flashes or night sweats, and any effects appear to be modest at best. It is not effective as a hormone treatment.

Wild Yam Extract
Claims that Yam has ‘body identical progesterone’ are unhelpful. The human body cannot make progesterone from yams. This is a myth. Wild yams (especially Dioscorea species) contain a plant compound called diosgenin. Diosgenin can be converted into progesterone in a laboratory, but human bodies cannot perform this conversion. The enzymes needed to turn diosgenin into progesterone do not exist in humans. That means eating yams does not raise progesterone levels, so “Yam progesterone” supplements do not work hormonally. Added to this, many over-the-counter “yam creams” contain no progesterone at all.
Animal hormones
Animal hormones are often sold as’ glandulars’ or ‘organ extracts’, or sometimes ovary, uterus, testis or adrenal supplements. They may be marketed as ‘natural hormone support’ or ‘endocrine nourishment’. To be clear, ‘hormone-boosting’ supplements made from cow or pig reproductive organs do not raise human hormone levels. Any actual hormones they contain are broken down during digestion, and what remains does not act as a hormone in the body.
Protein hormones (e.g. Luteinising Hormones - LH, Follicle-Stimulating Hormones - FSH and insulin) are broken down into amino acids by stomach acid and enzymes. Steroid hormones (e.g. oestrogen, progesterone, testosterone) are chemically fragile, present in only in tiny trace amounts, and largely inactivated during digestion. By the time a supplement reaches your bloodstream, there is no intact, biologically active hormone. Your endocrine system cannot “reassemble” hormones from digested fragments.
Hormones can be taken orally, but prescription-grade oral hormones are highly purified, given in precise, therapeutic doses and, most importantly, formulated to survive digestion and be absorbed. Oestrogen in hormone replacement therapy (HRT) is usually given via a patch or gel, rather than orally. Progesterone is usually given via a micronised pill or IUD device, and sometimes via patches.
The ones that got caught out
I had a look at whether any of these supplements have had their claims challenged. As these supplements are unregulated, this would normally be done via an advertising standards enforcement process, after someone lays a complaint. I found a few hits from the US, UK and New Zealand.
UK
In the UK, the Advertising Standards Authority (ASA) has ruled against Happy Koala’s MenoDaily, Feel Menopause Support, FemTech’s Key for Peri + Menopause, Feminapause, Napiers the Herbalists’ Wild Yam Cream, Rejuvit, Ovira and Dirtea.
In the case of Happy Koala (sold on the Happy Mammoth site), a Facebook advert claimed that the supplement could cure symptoms of menopause. It also made health claims that referred to a rate or amount of weight loss. Happy Koala said the ad had been shown in error, and that it had been removed from being shown to consumers in the UK. It feels a bit like they may be tailoring their advertising to include whatever claims they can get away with in each country until they get caught.
USA
In the US, the National Advertising Division (NAD) has ruled against Interceuticals’ BetterWOMAN supplement, Elements of Health Care’s L/Arginine Plus dietary supplements, Thermigen’s ThermiVa medical device, and Happy Mammoth’s Hormone Harmony Dietary Supplement.
In case you are wondering, ThermiVa is not a supplement - it’s a quick, non-invasive, non-ablative treatment delivering physician-controlled radiofrequency energy, using a thoughtfully designed handpiece to gently heat tissue.

Did you notice that’s the second time a ‘Happy Mammoth’ related company has come up? In August 2024, NAD recommended, as part of its routine monitoring program, that:
“Happy Mammoth discontinue certain health-related claims for its Hormone Harmony dietary supplement including that it “Relieves symptoms of Menopause”, “Relieves hot flashes”, “Improve sleep quality” and “Reduces bloating and gas”. Hormone Harmony contains a proprietary combination of ingredients, including fennel, chaste berry, ashwagandha, and chamomile, to ease menopausal discomfort.”

The National Advertising Division (NAD) determined that Happy Mammoth did not have a reasonable basis for the unqualified claims about the challenged benefits, as there had been no testing on the product itself. However, Happy Mammoth indicated a willingness to qualify the challenged claims to specify the efficacy of the ingredients in delivering the challenged benefits. NAD determined that the studies submitted by Happy Mammoth had limitations that rendered them insufficient to support the challenged claims, as well as the qualified claims and, therefore, recommended the claims be discontinued. NAD noted that:
nothing in its decision would prevent Happy Mammoth from:
- Making claims regarding the ability of fennel and chaste berry to positively affect menopausal symptoms that are supported by the limited findings of the research in evidence.
- Making supported claims that describe the traditional or historic use of ashwagandha to support sleep or are carefully qualified to avoid any misleading implication about the product’s efficacy or health benefits.
- Describing the traditional or historic use of chamomile in reducing bloating and gas.
Happy Mammoth agreed to voluntarily discontinue certain claims including “Relieves mood swings and boosts energy” and “Reduces … fluid retention.”
I feel like the NAD decision is almost endorsing some obtuse weaselly-worded health claims. Chaste berry, fennel, ashwagandha, and chamomile are not scientifically proven to relieve menopause symptoms. Evidence for their effectiveness is weak, limited, or indirect, with most studies showing no clear benefit over placebo. Additionally, their mechanisms of action and safety profiles are either not relevant to menopause, or not well-established.
In terms of the other ingredients in this supplement, there is no solid scientific evidence that rosemary, golden root, gymnema sylvestre leaf, or maca root effectively relieve menopause symptoms. Rosemary is mainly used for cooking, gymnema for blood sugar control, and maca’s support for menopause relies mostly on anecdotal reports and small studies, with no clear benefit for hot flashes or hormonal balance.
While most of these herbs are considered safe when used in moderation, several (especially black cohosh, ashwagandha, gymnema sylvestre, and rosemary at high doses) have been associated with rare but serious toxic effects in some individuals. People with underlying health conditions, those taking certain medications, and pregnant/breastfeeding women should exercise caution and consult a healthcare provider before using these supplements.
More details on the efficacy, and some potential side effects, of each of these herbs is included at the end of the article, for those who are interested in a more deep dive.
New Zealand
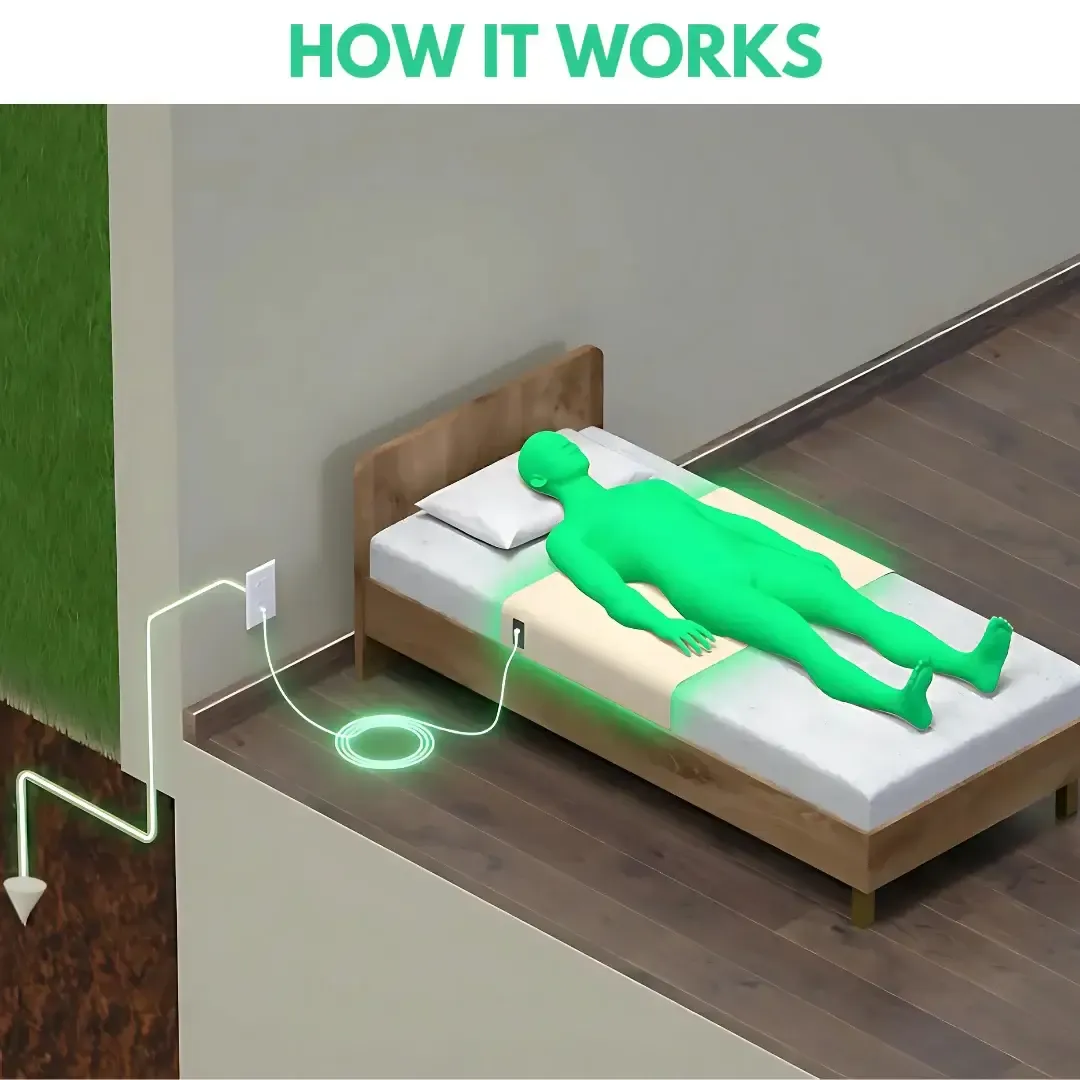
In New Zealand, we don’t see many complaints around menopause health claims at all. There is one finding that an outfit called ‘Premium Grounding’ made unsubstantiated therapeutic claims, including around menopause symptoms - but this was an earthing bed sheet, rather than a supplement. Grounding (or “earthing”) sheets are designed to conduct electricity so your body can be electrically connected to the earth while you sleep. They’re made from a mix of normal bedding materials and conductive elements - silver threads, carbon fibres, stainless steel fibres, etc. According to their website:
“Earthing works by allowing electrons to flow from the Earth into our bodies, neutralising free radicals and reducing oxidative stress. This process has been shown to: Reduce inflammation, improve sleep quality, Lower stress levels and cortisol production, Enhance cardiovascular health, Boost immune function, Accelerate recovery from exercise”
This sounds like a bunch of utter nonsense, but it’s out of the scope of this article.
So what’s up with the Mammoths?
The name that keeps coming up, ‘Happy Mammoth’, is an Australian-linked online supplement company selling products aimed at women, especially those going through perimenopause and menopause. It operates in Australia, the US, and the UK, and markets itself heavily on social media. It has been publicly slammed before for making exaggerated and false claims. Former menopause society leaders have described their adverts as “clever marketing nonsense”, and have said there’s no solid evidence that the supplements work as advertised.
The company runs thousands of ads on platforms like Facebook and Instagram, promising rapid weight loss and dramatic body changes without lifestyle changes. I have even had their ads pop up repeatedly on mobile games. Medical experts argue that the marketing preys on vulnerable women experiencing real symptoms and reinforces negative body stereotypes.
Independent customer reviews (e.g., on Trustpilot and other review sites) are mixed: some people report no benefits or negative experiences, and others feel the products didn’t do what was promised.
Conclusion
In summary, while a wide range of herbal supplements and alternative products are marketed as solutions for menopause symptoms, the available scientific evidence supporting their effectiveness is limited and often inconsistent. Marketing may exaggerate benefits while downplaying potential risks. Ultimately, informed decision-making and consultation with a doctor remains the best approach to managing menopause symptoms safely and effectively.
Popular supplement ingredients
Here is a summary of the information I found about some of the most popular menopause supplement ingredients. I’m not a medical professional, and this is not medical advice.
Ashwagandha - used in Ayurvedic medicine, ashwagandha is not scientifically proven to treat menopause symptoms. The evidence is limited and indirect. It may modulate cortisol and stress pathways, not oestrogen or progesterone directly. The long-term safety of ashwagandha is not known. While generally considered safe for most people at typical supplement doses, ashwagandha can cause gastrointestinal upset, diarrhoea, and vomiting. Rarely, cases of liver toxicity have been reported. It may interact with medications for thyroid, blood pressure, and immune function. Not recommended for people with autoimmune diseases, thyroid disorders, or those who are pregnant or breastfeeding.
Black Cohosh - Black cohosh is a highly popular herbal supplement, especially in the US, used primarily for alleviating menopausal symptoms like hot flashes. The Cochrane Review (2012) — looked at 16 randomized controlled trials (2,027 women) and found no significant benefit of black cohosh over placebo in reducing hot flash frequency or overall menopause symptom scores. The quality of the evidence was “uncertain and inconsistent”, so more research was recommended. A more recent meta-analysis reported that black cohosh extracts were associated with significant improvements in overall menopause symptoms and hot flashes compared with placebo, but with variability between studies and outcomes (e.g., no clear benefit for anxiety or depression). These analyses still don’t provide strong, consistent proof—results vary by study quality, formulation, and participant differences. Black cohosh has been associated with rare cases of liver toxicity, including hepatitis, liver failure, and jaundice. Individuals with liver disorders or those taking hepatotoxic medications should avoid it.
Chamomile - is not scientifically proven to treat menopause symptoms. Evidence is very limited and mostly anecdotal. It contains flavonoids and volatile oils that may have mild sedative or anti-inflammatory effects. Excessive use may cause nausea or vomiting.
Chaste berry - is not scientifically proven to help with menopause symptoms. The best evidence shows it helps premenstrual (PMS/PMDD) symptoms, not menopause. Chaste berry works mainly by acting on the dopamine system in the brain, which reduces prolactin levels. At best, this mechanism is relevant to PMS, breast tenderness and cycle-related mood symptoms. Not menopause. PMS and perimenopause are not the same thing! Chaste berry may cause gastrointestinal upset, headache, and skin reactions. It can interact with dopamine-related medications and hormonal therapies. Rarely, it may cause menstrual cycle disturbances.
Fennel - is also not scientifically proven to help with menopause symptoms. Evidence is very limited and low quality. Fennel contains phytooestrogens, plant compounds that weakly mimic oestrogen in lab studies. There are very limited human studies - mostly small trials or animal studies. The results of those studies are inconsistent. No controlled studies show a clear benefit over placebo. Fennel supplements may cause allergic reactions and, in rare cases, can interact with certain medications (especially those affecting hormones). Excessive intake could potentially be toxic due to high concentrations of certain plant compounds.
Golden root - There is no strong scientific evidence that golden root is effective for relieving menopause symptoms. While it is sometimes used for stress and fatigue, high-quality research specific to menopause symptom relief is lacking. Most available studies focus on its adaptogenic properties (helping the body resist and adapt to stress by normalising bodily functions, reducing fatigue, boosting immunity, and balancing hormones like cortisol) rather than hormonal balance or menopause-related symptoms. High doses may cause irritability, insomnia, or increased blood pressure.
Gymnema sylvestre - Gymnema sylvestre leaf has mainly been researched for its effects on blood sugar regulation and diabetes management. There is no quality evidence indicating that it is effective for relieving menopause symptoms. Gymnema can lower blood sugar, which may be dangerous for people taking diabetes medications. High doses may cause liver toxicity, though this is rare.
Maca root - Maca root is often marketed as a natural remedy for menopause symptoms, but current scientific evidence does not strongly support its effectiveness. While some small studies and anecdotal reports suggest that maca may help with energy, mood, or libido, high-quality research specifically investigating its impact on menopause symptoms such as hot flashes, night sweats, or hormonal balance is limited and inconclusive. Maca does not directly influence oestrogen or progesterone levels, which are key hormones involved in menopause.
Red Clover - Red clover is another herbal supplement often promoted for relief from menopausal symptoms, such as hot flashes. However, the scientific evidence supporting its effectiveness is mixed and generally considered weak. Some studies have suggested that red clover may have mild beneficial effects on hot flashes, but larger, more rigorous clinical trials have not consistently demonstrated significant improvements compared to placebo. The variability in results is attributed to differences in study design, formulations used, and participant characteristics. Red clover contains phytoestrogens and coumarins, which can interact with blood-thinning medications and hormone therapies. Large doses may increase risk of bleeding.
Rosemary - Rosemary is primarily used as a culinary herb and for its antioxidant properties, but there is no substantial scientific evidence to support its use for menopause symptom relief. Current research does not demonstrate benefits for hot flashes, night sweats, or other common menopause-related complaints. Very high doses of rosemary oil or extracts may be toxic, causing vomiting, spasms, or pulmonary edema.
St John’s Wort - There is some evidence St John’s wort may be beneficial for hot flashes, menopause-specific quality of life and sleep. However, these are small trials and doses of St John’s wort vary depending on the brand and preparation and there is no clear recommended dosage. Side effects include nausea or being sick, diarrhoea, headache, tiredness, dizziness, sleep difficulties. It can also cause skin allergies or reactions after sun exposure. Some people have experienced mania or psychosis. St John’s wort strongly affects liver enzymes which can lower the effectiveness of many medicines including antidepressants, oral contraceptives, HRT, blood thinners, anti seizure meds, immunosuppressants, HIV antivirals and cancer treatments. St John’s wort may also cause serious side effects if it is taken with other medicines. When combined with other antidepressants or serotonergic drugs (SSRIs, SNRIs, MAOIs, tramadol, triptans), it can cause a condition called serotonin syndrome which is a medical emergency.